www.drvaibhavshah.net
 |
| +Dr Vaibhav Shah |
 |
| +Dr Vaibhav Shah |
Eyebrows and eyelashes
make an important contribution to facial symmetry and presentation of self to
others. A person without eyebrows and/or eyelashes may feel very self-conscious
about his/her appearance. Transplantation or reconstructive surgery can often
restore eyebrows and eyelashes.
Eyebrows and eyelashes
are lost in a variety of ways:
·
Physical trauma—e.g.,
auto accident, thermal, chemical or electrical burns
·
Systemic or local
disease that causes loss of eyebrow and/or eyelashes
·
Congenital inability
to grow eyebrows and/or eyelashes
·
Plucking (to reshape
the eyebrow) that results in permanent loss of eyebrows
·
Self-inflicted
obsessive plucking or eyebrows and/or eyelashes (trichotillomania)
·
Medical or surgical
treatments that result in eyebrow or eyelash loss—e.g., radiation therapy,
chemotherapy, surgical removal of tumor.
The cause of
eyebrow/eyelash loss is evaluated in medical history and examination prior to
consideration of hair restoration:
·
Systemic or local
disease that causes hair loss must be under control to assure that hair
restoration can succeed
·
Obsessive-compulsive
plucking (trichotillomania) must be treated to assure that restored hair will
not be plucked out
·
Trauma, burns or
surgery may have resulted in formation of scar tissue; reconstructive surgery
may be necessary before eyebrow/eyelash restoration. The degree of eyebrow loss
may vary from complete to partial; the degree of loss may be a consideration in
selection of the restoration procedure.
Some patients have no
eyebrow/eyelash loss, but seek eyebrow/ eyelash enhancement for cosmetic
reasons such as a change in the shape of an eyebrow or longer eyelashes.
Eyebrow Hair
Restoration
A number of procedures
are available for restoration of all or part of the eyebrow:
Transplantation of
follicular units or single hairs from a donor area to the eyebrow, and a
reconstructive flap or graft procedure that brings a strip of hair from another
site to the eyebrow.
The patient and
surgeon must agree on the procedure best suited to the needs of the
patient. Eyebrow
restoration procedures are
usually performed in an outpatient setting. Postoperative complications are
usually limited to minor pain and swelling.
Reconstruction of the
Eyebrow Using Flaps or Grafts
Reconstructive surgery
has been used for many years to restore missing eyebrows or to repair partially
missing eyebrows. Technical considerations and the needs of the patient
determine which reconstructive procedure is used:
Transplants—Either a strip of hair-bearing skin and
subcutaneous tissue or individual follicular units by follicular unit
extraction (FUE) are removed from a donor area on the scalp, or donor areas on
the body, and grafted into the surgically-prepared eyebrow site. The transplant
procedure is performed by selecting a hair-bearing area of scalp with hair that
is of appropriate texture and orientation to serve as eyebrow hair. Follicular
units, usually of one to two hairs, are placed into incisions to achieve the
desired shape or density.
Scalp-to-eyebrow
pedicle flaps— (Less commonly used)
A strip of hair-bearing skin and subcutaneous tissue is raised from the temple
area just in front of the ear, with its blood supply (a branch of the
superficial temporal artery and vein) attached. This type of donor graft
attached to a blood supply is called a pedicle flap. After the pedicle flap is
raised, the recipient area (the eyebrow) is prepared to receive the flap. A
subcutaneous "tunnel" is created from the base of the pedicle flap to
the eyebrow recipient site; the flap is pulled through the tunnel and secured
to the recipient site with stitches. The pedicle flap’s blood supply nourishes
the grafted tissue until the grafted tissue develops its own blood supply from
surrounding tissue. Hairs grown from grafts and pedicles may have to be
"trained" with gel or wax to lay flat to the skin like eyebrow hair;
grafted hair will have to be trimmed occasionally.
Transplantation to
Correct Eyebrow Loss— One goal of
transplantation of hair to the eyebrow is to recreate the eyebrow in a natural
contour. The patient and physician must work together to outline the eyebrow
area to conform to the natural symmetry of the patient’s face. Depending on the
size of the area to be transplanted, more than one transplant session may be
required; two or more sessions several years apart are common.
As the transplanted
hairs grow in their new position they will require occasional trimming as well
as "training" with gel or wax.
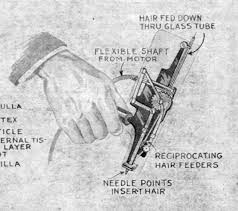
Eyelash Hair
Restoration (Eyelash Surgery)
Thin or short
eyelashes can be treated with Latisse however transplantation is the only
procedure used to restore eyelash hair when it has been lost. Eyelash surgery
is a very specialized procedure that is performed by just a few surgeons. As is
the case for eyebrows, donor hair for transplantation must be finer rather than
coarser. All grafts are single hairs meticulously placed into the lid. As few
as six hairs per lid may be adequate to create a natural effect.
Itching is a common
and troublesome postoperative complication. If the patient gives in to
temptation and scratches, there is risk for dislodging the hair grafts and
initiating infection. Eyeglasses may be worn to deter scratching. The
dermatologist can prescribe medications to relieve itching.
Training of
transplanted hairs into eyelash conformation is accomplished by use of lash oil
and an eyelash curler.